The diagnosis skin cancer hits those affected like a bolt from the blue. It is a diagnosis that is frightening and often leaves those affected and their family and friends in a state of helplessness. It is not only the uncertain health future that is frightening, but also the potentially high treatment costs associated with it.
Increase in skin cancer cases
In 2018, 287,723 cases of malignant skin cancer and 1,042,056 cases of non-malignant skin cancer were diagnosed worldwide. The numbers are steadily increasing year after year. For example, between 2008 and 2018, there was a 44% increase in skin cancer cases.
Top 5 countries with the highest incidence rate per capita
Statistically men are 10% more likely to develop melanoma skin cancer than women.
and also are 4% more likely to die from melanoma than women.
Every year, around 290,600 people in Germany are newly diagnosed with skin cancer. The number of diseases is increasing every year and now every third cancer diagnosis is skin cancer. In the UK, approximately 160,000 people are diagnosed with non-malignant skin cancer and 16,700 with malignant skin cancer each year.
Tissue removal (biopsy)
In order to be able to diagnose skin cancer, the suspicious tissue must be examined under the microscope – regardless of the type of skin tumour.
If the suspicion of melanoma is confirmed, the tumor is then removed completely with a safety margin, depending on the thickness of the tumor (excision). From a tumour thickness of 1 mm, the so-called sentinel lymph node is also removed.
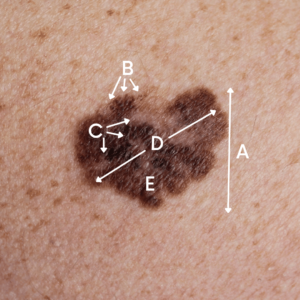
Tumor thickness - Breslow's depth
The thickness of skin cancer is differentiated between different T-classifications. The tumor thickness of the primary tumor in malignant melanoma is classified according to Breslow after surgical removal. This classification is the most important prognostic factor of malignant melanoma.
The larger the tumor thickness, the worse is the probable course of the disease and the chance of cure.
Safety distance for primary excision
After the malignant melanoma has been classified according to the tumor thickness, an excision is performed with a specific safety distance to the tumor margin, depending on the tumor thickness. This is extremely important to prevent the tumor from coming back.
Studies recommend a safety distance of 1 cm for a tumor thickness of 1-2 mm. For melanomas with a tumor thickness of 2 mm or more, a 2 cm safety distance should be made.
Before the surgical procedure, the surgeon should make the final decision for deviating
safety distances together with the patient. The localization of the tumor and the results of
the spread diagnostics should be taken into account.
Follow-up care
A standardized follow-up care over a 10-year period is an important component in the care of melanoma patients. The aim is to detect returning and secondary melanomas at an early stage.
Especially in the first 3 years after the primary diagnosis an intensive follow-up care should occur, since in this period 80% of returning malignant melanomas develop.
In addition, skin cancer patients should regularly and lifelong perform a self-examination of their skin for changes.
The follow-up care of melanoma patients should take place in risk-adapted and regular intervals.
Counselling centres
During this difficult time, affected persons and their relatives should not bear the entire burden of the diagnosis alone. For this reason, there is a nationwide network of cancer counselling centres in Germany.
There are also more than 60 Cancer Aid counselling centres in Austria. In the UK, the Macmillan Cancer Centre provides cancer patients with the support they need.
Summary
In summary, the earlier malignant melanoma is detected, the better the possible course of the disease and the chance of cure.
The correlation between early detection and tumor thickness is verifiable and also determines the safety margin for excision. In the early stages, skin cancer is easily treatable.
Through regular self-examination of the entire body, malignant and non-malignant skin cancer can be detected early. Remember, you are in your skin for life!
Sources:
2020 Melanoma UK Skin Cancer Report
Oncology guideline program (German Cancer Society, German Cancer Aid, AWMF): Diagnostics, therapy and follow-up of melanoma, long version 3.3, 2020, AWMF register number: 032/024OL, http://www.leitlinienprogrammonkologie.de/leitlinien/melanom/ (retrieved on: 10.11.2021).